After staring down the barrel of the largest cut to the Medicare home health payment rate ever proposed, home health providers are reacting to the final rule, announced on Friday. While the final rule included a 1.3% cut to aggregate Medicare payments to home health agencies, far short of the proposed 6.4% cut, home health […] The post ‘Doesn’t Cure The Illness’: Home Health Community Reacts To Medicare Final Rule appeared first on Home Health Care News.

This article is a part of your HHCN+ Membership
After staring down the barrel of the largest cut to the Medicare home health payment rate ever proposed, home health providers are reacting to the final rule, announced on Friday.
While the final rule included a 1.3% cut to aggregate Medicare payments to home health agencies, far short of the proposed 6.4% cut, home health stakeholders are balancing the good news with the bad. The cut will still reduce access to care, experts told Home Health Care News, and the methodology used to create the final rule remains in question.
Stakeholders say they will continue to push for change from Congress – or are asking CMS to reopen rulemaking.
On the whole, the home-based care community expressed dual feelings of tempered relief and a desire for greater change.
“While we acknowledge that CMS made significant adjustments in the Home Health Perspective Payment System Final Rule for CY 2026 in response to feedback from the Alliance and the care at home community, this cut will still have a negative impact on access to care at home,” Dr. Steve Landers, CEO of the National Alliance for Care at Home, told HHCN in an email.
Landers highlighted that Medicare home health providers have coped with reimbursement cuts since 2019, which has already reduced staffing, caused agency closures and reduced access to care.
The latest cut, while reduced from the proposed, continues this trend and adds pressure on providers.
“While we appreciate that CMS reduced the scale of its originally proposed cut, a $220 million reduction in Medicare home health payments still moves the industry in the wrong direction,” Justin Searle, practice president of home health at Bayada Home Health Care, told HHCN in an email. “For mission-driven providers like Bayada, each year of cuts makes it more challenging to recruit and retain nurses and caregivers, sustain services in rural and underserved communities and ensure patients who can be safely cared for at home continue to have access to that option.”
Pennsauken Township, New Jersey-based Bayada is a global nonprofit provider of home health care services.
Brent Korte, CEO of Dallas-based home health and hospice provider Frontpoint Health, lauded advocacy efforts from the home health industry and advocacy organizations.
“That said, although this is a relief for providers, clinicians, and patients, ultimately it doesn’t cure the illness the industry is dealing with: a gross underestimation of the value of care at home,” Korte told HHCN in an email. “I fear that until CMS, lawmakers, and payers realize the value of care in the home, the industry will be stuck in payment reform ‘Groundhog Day’.”
While the proposed rule amounted to a 9% cut to home health providers, the final rule amounts to a 4% cut, a “meaningful change,” according to a VNS Health statement shared with HHCN.
“But the final rule still results in a reduction for 2026 that brings cumulative cuts to nearly 14% since 2020, and saddles home health agencies with $4.7 billion in future reductions,” the company said. “At a time of rising labor costs, workforce shortages and increased patient complexity, these reductions seriously destabilize a benefit that millions of older adults rely on.”
New York City-based VNS Health is a nonprofit provider of home and community-based health care services.
G. Scott Herman, the founder and CEO of Fairview, Texas-based at-home care provider New Day Healthcare, called the finalized 1.3% aggregate cut a “rational decision.”
“Although we are happy CMS did take into consideration comments from providers and in making a rational decision around rates, we believe any reduction to home care limits for the elderly should be measured carefully,” Herman told HHCN in an email.
The rule’s effects
Though the final cut was far less drastic than the industry’s worst-case scenario, industry stakeholders still warn of the likely fallout of yet another cut to the home health payment rate.
Any cut to the home health payment rate impacts providers’ abilities to operate and serve older adults, according to Mollie Gurian, vice president of policy and government affairs at LeadingAge, the association of nonprofit providers of aging services, including home health.
“Our nonprofit, mission-driven members have already absorbed significant reductions since CY23 at a time when costs are rising, so even this “improved” figure adds pressure when agencies need more resources, not less,” Gurian told HHCN in an email. “Without Congressional intervention, these ongoing clawbacks will hang over the industry for years, limiting agencies’ ability to expand, invest in technology, and serve those who need care. It could even lead to mergers or closures.”
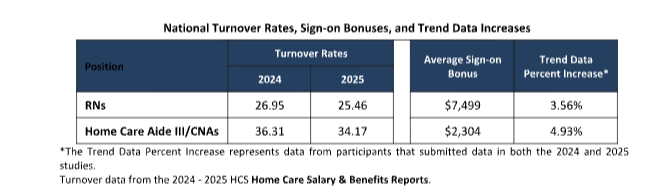
Continued rate cuts add pressure to an industry already afflicted with a labor crisis, according to Mike Asselta, CEO of Compassus.
“Labor and benefits comprise the largest portion of costs for providers, with annual wage growth reflecting the value and dedication of care teams,” Asselta told HHCN in an email. “Unfortunately, Medicare’s declining reimbursement rates threaten the financial viability of a workforce critical to delivering this meaningful care. These cuts are especially difficult to reconcile given the demonstrated value of home health services to both the Medicare trust and its beneficiaries.”
Brentwood, Tennessee-based Compassus provides home health, home infusion, palliative and hospice care services.
Bayada does not anticipate a “single drastic change on a specific date” because of cut included in the final rule, but the organization will continue to adopt technologies that ease documentation burden and reduce hospital readmissions and other adverse outcomes.
Additionally, Searle said Bayada would continue to evaluate its organizational structure to prioritize resources for frontline workers. In June, the organization laid off 10% of its headquarters staff, citing reimbursement challenges.
The methodology
Home health stakeholders also called CMS’ algorithm for determining the Medicare payment rate – a topic that was brought up repeatedly during the proposed year’s public comment period.
“The true problem lies in how CMS sets payment rates, using assumptions and analyses that don’t reflect what’s actually happening in the field and making the system easier for bad actors to exploit,” VNS Health said. “As a result, payments fall short of the true cost of care, making it even harder for older adults to get the home health support they need.”
CMS’ decision-making process was improved from that of the proposed rule, according to Landers.
“We commend CMS for revisiting aspects of its seriously flawed payment proposal, including the conclusion of permanent payment adjustments with CY 2026 (using data from CY 2020 through 2022) based on issues that CMS acknowledged with isolating PDGM behavior changes from non-PDGM behavior changes in CYs 2023 and beyond,” Landers said.
“However, while CMS reduced the amount of overpayments that inform the temporary payment adjustments down to 4.7 billion for CYs 2020 through 2024, home health agencies will continue to face several more years of temporary adjustments without additional action,” he continued.
Commenters on the proposed rule often said that CMS should target agencies committing billing fraud – like a notable example in California – rather than implement a blanket decrease to the home health payment rate. Other comments focused on other aspects of the organization’s methodology, including that cost reports were not representative of the actual costs of care.
CMS responded to these comments in the final rule, saying that its methodology trims out the top or bottom 1% of all home health agencies’ cost report data in order to cull questionable data. The organization also said that further trimming is not possible under its current policy.
“Not all anomalous billing patterns indicate fraudulent practice, and we would need further evidence to determine which providers with anomalous billing patterns can be connected to fraudulent practices,” the final rule read. “Excluding data some commenters view as “anomalous” from the calculation of the national 30-day base payment rate, would thus require CMS to develop a new policy, including thresholds for determining deviations excluded from the analytical sample.”
An AccentCare spokesperson told HHCN that CMS’ failure to exclude anomalous or fraud-tainted claims allows “distorted data to continue influencing national payment rates.”
Dallas-based AccentCare is a provider of personal care, home health, palliative care and hospice services.
Next steps
Providers and advocacy groups called on Congress to take action to protect the Medicare home health benefit.
Systematic policy change is necessary to ensure access to home health care, Asselta said.
“We appreciate the willingness of CMS to mitigate its proposed cuts to home health services,” Asselta said. “Having said that, we urge CMS to reevaluate its decision and eliminate all rate cuts, keeping its promise to seniors and the Medicare trust at the forefront.”
Stakeholders, including AccentCare and VNS Health, called on CMS to reopen rulemaking and update its methodology.
Providers and the Alliance have pinned some hope on the Home Health Stabilization Act of 2025. The bill would pause cuts to the Medicare home health reimbursement rate for 2026 and 2027 and provide time to “look deeper under the hood at how this has happened,” Scott Levy, chief government affairs officer at the Alliance, previously told HHCN.
“We cannot stand still with home health facing these misguided cuts,” Landers said. “Congress has an essential role to play in ensuring long-term stability and preserving access to high-quality home health care. We are urging further action to support and strengthen home-based care, which is among the most trusted, cost-effective and patient-centered services in the Medicare program.”
The post ‘Doesn’t Cure The Illness’: Home Health Community Reacts To Medicare Final Rule appeared first on Home Health Care News.